2024-10-22
Our group has made progress in the treatment of myocardial infarction with biomaterials
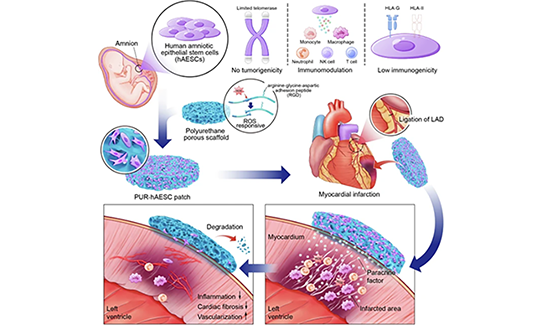
Myocardial infarction (MI) is a serious risk to human health and imposes a significant economic burden on society. Current clinical treatments are limited and fail to address irreversible myocardial necrosis and cardiac function decline. Therefore, new therapeutic strategies need to be developed urgently. MI stem cell therapy, represented by embryonic stem cells and induced pluripotent stem cells, has developed rapidly in recent years, mainly targeting the replacement supplementation of damaged and dead cardiomyocytes. Although this strategy has achieved some success, the varying degree of differentiation of transplanted cardiomyocytes, low integration rate, low survival rate, and abnormal electrophysiological and mechanical functions of the repaired heart pose a series of challenges, in addition to tumorigenicity, immune rejection, and ethical issues. Recently, it has been proposed in Nature and other journals that alteration of the inflammatory environment is crucial for MI repair, and the key mechanism of stem cell transplantation to intervene in MI is likely to be through modulation of the microenvironment of the injured tissue. Therefore, the development of clinically applicable stem cell therapeutic regimens for MI pathologic microenvironment modulation will provide a more effective intervention strategy for MI treatment.On October 22, 2024, Luyang Yu's team from School of Life Sciences, Zhejiang University and Changyou Gao's team from Department of Polymer Science and Engineering, Zhejiang University jointly published a paper titled “Epicardial transplantation of antioxidant polyurethane scaffold based stem cell therapy” in Nature Communications. Epicardial transplantation of antioxidant polyurethane scaffold based human amniotic epithelial stem cell patch for myocardial infarction treatment” in Nature Communications. The study reported the construction of functional cardiac patch of antioxidant polyurethane scaffold based human amniotic epithelial stem cell for myocardial infarction treatment, its therapeutic effect on MI and the mechanism of microenvironmental regulation in infarcted area, which provided a new idea for the clinical treatment of MI.In previous study, it's found that human amniotic epithelial stem cells (hAESCs) have strong paracrine and immunomodulatory effects, etc., and they have good biosafety with low immunogenicity, no tumorigenicity and ethical issues. In this study, in order to solve the problem of low cell retention and survival, ROS-responsive polyurethane porous patch (PUR) was used as a delivery vehicle for hAESCs, which not only provides mechanical support for the transplanted cells, but also “intelligently” mitigates oxidative stress in the tissue microenvironment, prevents ischemic damage and inflammation, and protects their viability and function. It can also “intelligently” mitigate oxidative stress in the tissue microenvironment, prevent damage such as ischemic injury and inflammation, and protect their viability and function. The researchers optimized the material design to obtain porous antioxidant polyurethane (PUR) scaffolds with good biocompatibility, and then constructed engineered multifunctional stem cell cardiac patches using hAESCs as seed cells. Subsequently, a rat infarction model was utilized to explore the multifaceted roles of hAESCs-PUR patches in regulating the microenvironment in the context of myocardial injury by combining single-cell sequencing and other methods. In the rat model, PUR-hAESC patch significantly reduced myocardial fibrosis and promoted myocardial angiogenesis after myocardial infarction, thereby improving cardiac function and cardiac remodeling (Figure 1). Mechanistic studies revealed that PUR-hAESC patch significantly inhibited the invasion of neutrophils and specific inflammatory macrophage subpopulations (Hif1α+, Spp1+) in the myocardial infarction zone, and suppressed the expression of pro-inflammatory factors (IFN-γ, TNF-α).Figure 1: PUR-hAESC patch improves ventricular dysfunction and reduces pathologic cardiac remodeling after MI.In summary, this study established a comprehensive strategy for myocardial injury repair that integrates mechanical support, “smart” ROS scavenging, immune remodeling, and paracrine modulation, providing a potential clinical treatment strategy for myocardial infarction (Figure 2).Figure 2: Schematic diagram of PUR-hAESC cardiac patch for myocardial infarction.This study was conducted by the team of Prof. Luyang Yu from the School of Life Sciences, Zhejiang University in collaboration with the team of Prof. Changyou Gao and Yang Zhu from the Department of Polymer Science and Engineering, Zhejiang University. Jinying Li, Distinguished Researcher of ZJU-Lishui Joint Innovation Center for Life and Health, and Yuejun Yao, a 2022 PhD student of the Department of Polymer Science and Engineering of ZJU, are the co-first authors, while Prof. Luyang Yu, Prof. Changyou Gao, and Prof. Yang Zhu, a long-time Associate Professor, are the co-corresponding authors, and PhD student Chia-Yi Zhou, M.S. student Zhuoheng Yang, and other members of the team of the Department of Polymer Science and Engineering of the School of Life Sciences of Zhejiang University are the co-first authors of this paper. This work was supported by the Leading Goose Project of Zhejiang Key R&D Program, National Key R&D Special Project, National Natural Science Foundation of China, and the Space Science and Application Project of National Manned Space Station Engineering.Link to original article:https://www.nature.com/articles/s41467-024-53531-8